Pfizer and BioNTech’s coronavirus vaccine inched a step closer toward approval on Monday, with the company announcing 90% efficacy in phase 3 clinical trial. The vaccine will be offered in a two-dose jab, not unlike other candidates currently in development and a multitude of multi-dose medicines that have come before it. The vaccine’s two doses will be separated by a period of 21 days, with the first shot occurring on day zero, Dr. Anuj Mehta, a pulmonary and critical care physician at National Jewish Health, explained to Fox News. The period between the two shots is based on data collected in the lab before the vaccine was tested in humans, he explained. Each dose will be comprised of the same formulation, meaning there is no difference between the shots, but the reason there has to be two is because the body responds to each differently. The first dose, Mehta said, acts as a primer for the body’s immune system, and the second dose, given three weeks later, will kick it into gear, so to speak. Mehta, a member of the medical advisory group of the Governor’s Expert Emergency Epidemic Response Committee in Colorado who is not involved in Pfizer’s trials, said after the second dose the body will be able to better recognize the proteins created by the COVID-19 virus, translating into immunity. How long that immunity lasts, however, remains to be seen. “Based on the press release from Pfizer, it appears that the immunity sets in within a week of the second dose,” Mehta said, citing the press release published by Pfizer. “All the data supports the fact that a single-dose won’t provide really robust immunity, which is what we need to combat the pandemic.” Mehta added that it’s too soon to know if the vaccine will be an annual inoculation, similar to the flu shot, or if it will be effective for several years. “We don’t know if this is going to be something where people need repeated immunizations at different time intervals, or it’ll be sufficient for a very long period of time,” he said. “Long-term follow up included with the trials will tell us that.
Record Infections Death Rates and it getting worse by the day
Several states posted records Tuesday, including over 12,600 new cases in Illinois, 10,800 in Texas and 7,000 in Wisconsin.
Deaths — a lagging indicator, since it takes time for people to get sick and die — are climbing again, reaching an average of more than 930 a day.
Hospitals are getting slammed. And unlike the earlier outbreaks, this one is not confined to a region or two.
“The virus is spreading in a largely uncontrolled fashion across the vast majority of the country,” said Dr. William Schaffner, an infectious-disease expert at Vanderbilt University.
Governors made increasingly desperate pleas for people to take the fight against the virus more seriously.
In an unusual prime-time speech hours after Wisconsin set new records for infections and deaths, Democratic Gov. Tony Evers announced that he was advising people to stay in their houses and businesses to allow people to work remotely, require masks and limit the number of people in stores and offices.
Minnesota Gov. Tim Walz, a Democrat, ordered bars and restaurants to close at 10 p.m., and Iowa Gov. Kim Reynolds, a Republican, said she will require masks at indoor gatherings of 25 or more people, inching toward more stringent measures after months of holding out.
While deaths are still well below the U.S. peak of about 2,200 per day back in April, some researchers estimate the nation’s overall toll will hit about 400,000 by Feb. 1, up from about 240,000 now.
But there is also some good news.
Doctors now better know how to treat severe cases, meaning higher percentages of the COVID-19 patients who go into intensive care units are coming out alive. Patients have the benefit of new treatments, namely remdesivir, the steroid dexamethasone and an antibody drug that won emergency-use approval from the Food and Drug Administration on Monday. Also, testing is more widely available.
In addition, a vaccine appears to be on the horizon, perhaps around the end of the year, with Pfizer this week reporting early results showing that its experimental shots are a surprising 90% effective at preventing the disease.
And there’s a change pending in the White House, with President-elect Joe Biden vowing to rely on a highly respected set of medical advisers and carry out a detailed coronavirus plan that experts say includes the kind of measures that will be necessary to bring the surge under control.
Biden pledged during the campaign to be guided by science, make testing free and widely available, hire thousands of health workers to undertake contact-tracing, and instruct the Centers for Disease Control and Prevention to provide clear, expert advice.
“We are already seeing encouraging signs from President-elect Biden with regard to his handling of COVID-19,” said Dr. Kelly Henning, a veteran epidemiologist who heads the Bloomberg Philanthropies’ public health programs.
“I am relieved to see he’s already put some of the smartest scientific minds on his new coronavirus task force and that they are acting urgently to try and get the pandemic under control as quickly as possible,” Henning said.
While the first surge in the Northeast caught many Americans unprepared and cut an especially deadly swath through nursing homes, the second crest along the nation’s Southern and Western rim was attributed mostly to heedless behavior, particularly among young adults over Memorial Day and July Fourth, and hot weather that sent people indoors, where the virus spreads more easily.
The fall surge similarly has been blamed largely on cold weather driving people inside and disdain for masks and social distancing, stoked by President Donald Trump and other politicians.
Even in parts of the country that have been through coronavirus surges before, “you see people breaking out of it” and letting their guard down, Schaffner said.
“There really is COVID fatigue that is blending into COVID annoyance,” he said.
The short-term outlook is grim, with colder weather and Thanksgiving, Christmas and New Year’s ahead. Generations of family members gathering indoors for meals for extended periods “is not a recipe for anything good,” Hanage said.
Other factors could contribute to the spread of the virus in the coming weeks: Last weekend saw big street celebrations and protests over the election. On Saturday night, an upset victory by Notre Dame’s football team sent thousands of students swarming onto the field, many without masks.
Meanwhile, the next two months will see a lame-duck Congress and a president who might be even less inclined than before to enact disease-control measures. Those voted out of office or no longer worried about reelection for at least two more years, “are not going to be motivated to do a fantastic job,” Hanage said.
Experts are increasingly alarmed about the virus’s resurgence in places like Massachusetts, which has seen a dramatic rise in cases since Labor Day, blamed largely on young people socializing.
Republican Gov. Charlie Baker is warning that the health care system could become overwhelmed this winter, and he recently ordered restaurants to stop table service, required many businesses to close by 9:30 p.m., and instructed residents to stay home between 10 p.m. and 5 a.m.
Brooke Nichols, a professor and infectious-disease mathematical modeler at Boston University School of Public Health, said the governor’s actions don’t go far enough.
“Right now because of the exponential growth, throw the kitchen sink at this, and then you can do it for not as long,” Nichols said.
Meanwhile, political leaders in a number of newer coronavirus hot spots are doing less. In hard-hit South Dakota, Gov. Kristi Noem has made it clear she will not institute a mask requirement and has voiced doubt in health experts who say face coverings prevent infections from spreading.
Even higher case and death rates have been seen in North Dakota, where many people have refused to wear masks. Gov. Doug Burgum has pleaded with people to do so, and praised local towns and cities that have mandated masks. But he has avoided requiring masks himself.
Both Noem and Burgum are Republicans and have taken positions in line with those of the president.
“It would be simplistic to say it’s a red-vs.-a-blue experience, but it does kind of go along party lines of whether people took it seriously, tried to prevent it and took painful measures, versus those who said, ‘Let it rip,’” said Dr. Howard Markel, a public health historian at the University of Michigan.
___
Associated Press writer Alanna Durkin Richer in Boston contributed to this report.
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Department of Science Education. The AP is solely responsible for all content.
US hits record COVID-19 hospitalizations amid virus surge
NEW YORK (AP) — The U.S. hit a record number of coronavirus hospitalizations Tuesday and surpassed 1 million new confirmed cases in just the first 10 days of November amid a nationwide surge of infections that shows no signs of slowing. The new wave appears bigger and more widespread than the surges that happened in the spring and summer — and threatens to be worse. But experts say there are also reasons to think the nation is better able to deal with the virus this time around. “We’re definitely in a better place” when it comes to improved medical tools and knowledge, said William Hanage, a Harvard University infectious-disease researcher. Newly confirmed infections in the U.S. were running at all-time highs of well over 100,000 per day, pushing the total to more than 10 million and eclipsing 1 million since Halloween. There are now 61,964 people hospitalized, according to the COVID Tracking Project.
Several states posted records Tuesday, including over 12,600 new cases in Illinois, 10,800 in Texas and 7,000 in Wisconsin. Deaths — a lagging indicator, since it takes time for people to get sick and die — are climbing again, reaching an average of more than 930 a day. Hospitals are getting slammed. And unlike the earlier outbreaks, this one is not confined to a region or two. “The virus is spreading in a largely uncontrolled fashion across the vast majority of the country,” said Dr. William Schaffner, an infectious-disease expert at Vanderbilt University. Governors made increasingly desperate pleas for people to take the fight against the virus more seriously. In an unusual prime-time speech hours after Wisconsin set new records for infections and deaths, Democratic Gov. Tony Evers announced that he was advising people to stay in their houses and businesses to allow people to work remotely, require masks and limit the number of people in stores and offices. Minnesota Gov. Tim Walz, a Democrat, ordered bars and restaurants to close at 10 p.m., and Iowa Gov. Kim Reynolds, a Republican, said she will require masks at indoor gatherings of 25 or more people, inching toward more stringent measures after months of holding out. While deaths are still well below the U.S. peak of about 2,200 per day back in April, some researchers estimate the nation’s overall toll will hit about 400,000 by Feb. 1, up from about 240,000 now.
A vaccine appears to be on the horizon, perhaps around the end of the year, with Pfizer this week reporting early results showing that its experimental shots are a surprising 90% effective at preventing the disease. While the first surge in the Northeast caught many Americans unprepared and cut an especially deadly swath through nursing homes, the second crest along the nation’s Southern and Western rim was attributed mostly to heedless behavior, particularly among young adults over Memorial Day and July Fourth, and hot weather that sent people indoors, where the virus spreads more easily. The fall surge similarly has been blamed largely on cold weather driving people inside and disdain for masks and social distancing, stoked by President Donald Trump and other politicians. Even in parts of the country that have been through coronavirus surges before, “you see people breaking out of it” and letting their guard down, Schaffner said.
Other factors could contribute to the spread of the virus in the coming weeks: Last weekend saw big street celebrations and protests over the election. On Saturday night, an upset victory by Notre Dame’s football team sent thousands of students swarming onto the field, many without masks. Meanwhile, the next two months will see a lame-duck Congress and a president who might be even less inclined than before to enact disease-control measures. Those voted out of office or no longer worried about reelection for at least two more years, “are not going to be motivated to do a fantastic job,” Hanage said.
Experts are increasingly alarmed about the virus’s resurgence in places like Massachusetts, which has seen a dramatic rise in cases since Labor Day, blamed largely on young people socializing.
Republican Gov. Charlie Baker is warning that the health care system could become overwhelmed this winter, and he recently ordered restaurants to stop table service, required many businesses to close by 9:30 p.m., and instructed residents to stay home between 10 p.m. and 5 a.m. Brooke Nichols, a professor and infectious-disease mathematical modeler at Boston University School of Public Health, said the governor’s actions don’t go far enough. “Right now because of the exponential growth, throw the kitchen sink at this, and then you can do it for not as long,” Nichols said. Meanwhile, political leaders in a number of newer coronavirus hot spots are doing less. In hard-hit South Dakota, Gov. Kristi Noem has made it clear she will not institute a mask requirement and has voiced doubt in health experts who say face coverings prevent infections from spreading. Even higher case and death rates have been seen in North Dakota, where many people have refused to wear masks. Gov. Doug Burgum has pleaded with people to do so, and praised local towns and cities that have mandated masks. But he has avoided requiring masks himself.
‘Great day for humanity’: Pfizer says COVID-19 vaccine over 90% effective
(Reuters) – Pfizer Inc’s PFE.N experimental COVID-19 vaccine was more than 90% effective based on initial trial results, the company said on Monday, a major victory in the fight against a pandemic that has killed over a million people and battered the world’s economy.Experts welcomed the first successful interim data from a large-scale clinical test as a watershed moment that showed vaccines could halt the pandemic though mass roll-outs of the shot, which needs regulatory approval, won’t happen this year. Pfizer and its German partner BioNTech SE BNTX.O said they had so far found no serious safety concerns and expected to seek U.S. authorization this month for emergency use of the vaccine, raising the possibility of a regulatory decision as soon as December. If granted, the companies estimate they can roll out up to 50 million doses this year, enough to protect 25 million people, and then produce up to 1.3 billion doses in 2021. “Today is a great day for science and humanity,” Albert Bourla, Pfizer’s chairman and chief executive, said. “We are reaching this critical milestone in our vaccine development program at a time when the world needs it most with infection rates setting new records, hospitals nearing over-capacity and economies struggling to reopen.” Experts cautioned that they still needed to see the full trial data, which have yet to be peer-reviewed or published in a medical journal, but the preliminary results looked encouraging so far. There are still many questions around the vaccine, such as how effective it is for vulnerable groups and how long it will provide immunity, and the “new normal” of social distancing and face masks looks set to remain for the foreseeable future. BioNTech Chief Executive Ugur Sahin told Reuters he was optimistic the immunisation effect of the vaccine would last for a year though that was not yet certain. “This news made me smile from ear to ear. It is a relief to see such positive results on this vaccine and bodes well for COVID-19 vaccines in general,” said Peter Horby, professor of emerging infectious diseases at the University of Oxford. The prospect of a vaccine electrified world markets with the S&P 500 and Dow hitting record highs as shares of banks, oil majors and travel companies soared. Pfizer shares were 8.6% higher in New York at 1450 GMT, while BioNTech’s stock was up 11%.
More nurses dead from coronavirus than in WWI – Int’l Council of Nurses
An independent investigation probes the death toll of healthcare workers, estimating it is much higher than reported, and condemns worldwide organizations for not doing as such.

An independent investigation probes the death toll of healthcare workers, estimating it is much higher than reported, and condemns worldwide organizations for not doing as such.The International Council of Nurses is a federation that represents more than 20 million nurses worldwide. When they conducted their own data analysis, they discovered that 1,500 nurses have died so far from COVID-19. Up from 1,097 in August, that’s the highest nurse-death count since World War I, the ICN announced on Wednesday, October 28.
Is the COVID-19 risk on airplanes really that low? Here’s what experts say

With the demand for air travel still in a slump, the airline industry is promoting studies that suggest the risk of contracting the coronavirus while flying is low. Although healthcare experts say the air filtration system in most commercial planes helps reduce the risk of being infected, they point out that the studies have limitations and the results are not all definitive.
Delta Air Lines and two of the world’s largest airline-industry trade groups have promoted the recent studies as they seek to ease the fear of flying during a pandemic that has killed more than a million people worldwide.
New study from @HarvardChanSPH reveals that the multiple layers of protection against COVID-19 make being on an airplane as safe if not substantially safer than other routine activities, such as grocery shopping or going to a restaurant. https://t.co/HG8l0ep2UD
— Airlines for America (@AirlinesDotOrg) October 28, 2020
Why is it important to airlines to promote the safety of flying?
The volume of passengers flying on U.S.-based airlines is down 63% compared with the same time last year, with domestic travel dropping 61% and international flying down 77%. As a result, U.S.-based carriers are losing more than $200 million a day combined, according to Airlines for America, a trade group for the U.S. airline industry.
What are the studies they’re promoting?
The most prominent study was conducted and sponsored by United Airlines, airplane manufacturer Boeing and the U.S. Department of Defense. To see how the coronavirus might spread in a commercial jet, the study measured a fluorescent aerosol spray that was emitted from a mannequin placed in various seats in two types of Boeing jets.
The mannequin was moved throughout the cabins of the planes, with sensors installed in surrounding seats to measure how far the aerosol spray traveled. More than 300 tests were conducted, with variables such as having the mannequin emit aerosol at different strengths to replicate breathing, speaking or coughing. Tests were performed with and without the mannequin wearing a mask.
The study concluded that the “aerosol exposure risk is minimal even during long duration flights,” with the highest risk coming to those sitting in the same row as the mannequin.
Do healthcare experts agree?
Only partially. Infectious-disease and healthcare experts say the study correctly concludes that the infection risk is lower on a plane than in places such as stores and restaurants. The study gave much of the credit to the air circulation system in airplane cabins that pushes air through high-efficiency particulate air filters, known as HEPA filters.
But the experts note that the test was limited to certain scenarios. The study did not measure what happens when an infected passenger turns his or her head to talk to a fellow traveler or gets out of the seat to walk down the aisle or use the lavatory. The mannequin stayed in a seat, facing forward, during the tests. “In real life, people move around the plane, disrupting the airflow and probably resulting in higher exposures in some locations and lower exposures in others, compared to the study,” said Linsey Marr, a professor of civil and environmental engineering at Virginia Tech. “These real-life considerations could easily increase the risk by a factor of 10 to 100.” The test also assumed that all passengers wore masks and that the cabin had only one infected person.
Mercedes Carnethon, a professor of preventive medicine at Northwestern University, added that the study did not gauge the risk of getting to and from a flight, walking through a crowded airport terminal and queueing up with travelers who may or may not be wearing masks.
“Based on these findings, the time spent on the airplane is not the riskiest aspect of traveling,” she said. The study includes a section titled “Limitations and Assumptions” that acknowledges some of those points.
What other data have been touted by the airline industry?
The International Air Transport Assn., the trade group for the world’s airlines, announced this month that there have been only 44 cases this year in which COVID-19 is believed to have been transmitted on a plane. By comparison, the group noted, about 1.2 billion travelers have flown on commercial flights worldwide in the same period.
“We think these figures are extremely reassuring,” Dr. David Powell, the IATA’s medical advisor, said in a statement. “Furthermore, the vast majority of published cases occurred before the wearing of face coverings in flight became widespread.”
The group said its numbers align with data in a study recently published in the Journal of Travel Medicine.
Is everyone on board with that?
No. Dr. David O. Freedman, a professor emeritus of infectious disease at the University of Alabama at Birmingham who co-wrote the Journal of Travel Medicine study, said the IATA misrepresented his findings.
Although he agrees that the overall risk of getting infected while in a plane is low, he said the IATA cannot assume that only 44 travelers have been infected on flights when there are no data showing that the other 1.2 billion fliers were tested or quarantined after they disembarked from their flights.
“You can’t say the denominator is 1.2 billion uninfected because only a small handful of these passengers were ever tested for COVID,” Freedman said. “IATA wanted a number, but no good published risk numbers are yet out there.”
In the Oct. 8 press release that touted its findings, the IATA acknowledged that “there is no way to establish an exact tally of possible flight-associated cases.” It said it reached out to airlines and public health authorities and reviewed available literature and found no “indication that onboard transmission is in any way common or widespread.”
Are there other industry-backed studies?
The Harvard T.H. Chan School of Public Health released a study Tuesday that was sponsored by Airlines for America and a consortium of other airline businesses that concluded “there has been little evidence to date of onboard disease transmission.” The study was based on the review of previously published studies and public data, plus modeling of onboard disease transmission data conducted by Harvard experts. The study said airlines have kept onboard transmissions low by requiring masks on all passengers and crew members, pushing cabin air through HEPA filters, disinfecting cabins between flights and screening passengers for COVID-19 symptoms.
Did the study call for any changes in the way we fly?
The Harvard study concluded that to further reduce the risk of onboard infections, airlines should continue to operate the air ventilation system while passengers are boarding and leaving the plane. It also said passengers should be encouraged to maintain physical distance from one another when they file into the plane’s cramped aisles to find their seats and when filing out to exit the plane.
US sees record 88,521 new daily virus cases
The U.S. has reported a record-breaking number of new coronavirus cases, continuing an alarming surge and stoking concerns from health experts that the nation could be in for a difficult winter. The country reported 83,757 new Covid-19 cases on Friday, passing the last record of roughly 77,300 cases seen on July 16 as the U.S. grappled with outbreaks in Sun Belt states, according to data compiled by Johns Hopkins University. On Saturday, the U.S. reported another 83,718 new coronavirus cases. “I think we’re in for a very hard stretch here,” Dr. Scott Gottlieb, the former U.S. Food and Drug Administration commissioner, told CNBC on Friday evening. “I think the winter is going to be very difficult.”

Coronavirus cases grew by 5% or more over the past week in 37 states as of Friday, according to a CNBC analysis of Johns Hopkins data that uses a weekly average to smooth out fluctuations in daily reporting. Some states, like California and Alabama, have been working through a backlog of tests that were added to Friday’s count, pushing the nation’s total higher, according to their data dashboards. However, the nation is now reporting roughly 63,200 daily new cases based on a weekly average, a more than 14% increase compared with a week ago. While Covid-19 testing is up nearly 13% from Oct. 1, new cases have risen at a much faster rate. The seven-day average of new infections is up 51% over that same period, according to Johns Hopkins data. “I think we’re going to bear a lot more infection … and the health-care system is going to have to bear the brunt of this burden, because I don’t think you have the popular will for stay-at-home orders or broad mitigation,” Gottlieb said, adding that the virus’ spread would slow “if everyone would just wear masks.” The recent surge is a “distressing trend” that is likely due to “smaller, more intimate gatherings of family, friends and neighbors” that are moving indoors as the weather cools, Jay Butler, the U.S. Centers for Disease Control and Prevention’s deputy director for infectious diseases, told reporters on a conference call Wednesday. The outbreaks are building throughout the country with particular areas of concern in the Midwest, Butler said. As of Friday, North Dakota, South Dakota, Montana and Wisconsin continue to report the highest number of new cases per capita.

The increase in cases in several states are leading to more hospitalizations and will ultimately lead to more deaths, White House coronavirus advisor Dr. Anthony Fauci told MSNBC’s Chuck Todd on Friday. Thirteen states reached record high hospitalizations on Friday, based on a weekly average. Many of them are in the West and Midwest, including Iowa, Montana, North Dakota, Nebraska, Ohio, Oklahoma, South Dakota, Utah, Wisconsin and Wyoming, according to a CNBC analysis of Covid Tracking Project data. Coronavirus deaths have remained relatively flat in the U.S., though health experts warn fatalities typically lag infections by a few weeks. “When you enter the season of the cooler months of the fall and the colder months of the winter, where a lot of activity, out of necessity, is going to be inside as opposed to outside, that’s a difficult and challenging situation to be in because you have a couple of factors against you,” Fauci said.

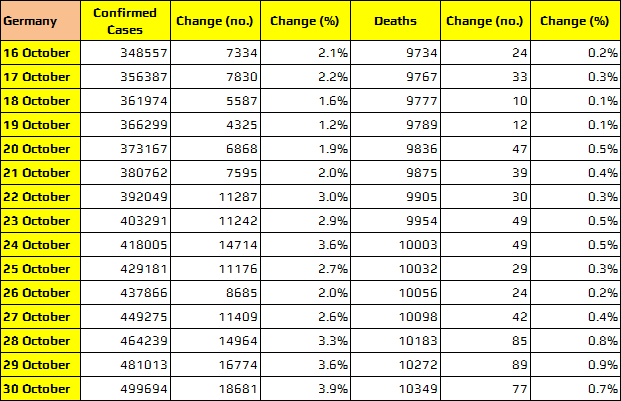
Germany adds record 18,681 COVID cases, 77 deaths
Salvavida Suggestions
Salvavida Suggestions:
- Isolation from people is the BEST thing you can do. For people I must see they stay OUTSIDE and we speak through Plexiglas.
- Constantly circulate your air. I suck in air through a panel ULPA U15 clean room filter I made and I exhaust the air through a powered ventilator on the roof. We’re in the process of looking into manufacturing ULPA U15 clean room/biolab filters for your air conditioning and forced air systems. If you have an interest, contact us at 866-924-0607 with the size of your present filters.
- Use a proper reusable surgical silicone mask (we still have some in stock) with P3 U15 filters. I exhausted all supplies of workable P3 cartridge filters. SO I made my own. They are the ONLY P3 R ULPA U15 cartridge filters made in the world for face masks (click here to see specifications). I took the technology from Biolabs Level 4 filtration systems. If you had showed an interest I sent you a complimentary sample of my new cartridge filter.
- I take Vitamin D3 in the form of Choleciferol. Usually that is a minimum of 10,000 IU a day. Studies have shown you should raise your blood levels to 25(OH)D concentrations above 40–60 ng/mL (100–150 nmol/L). You can only know by getting your blood tested. I do blood tests every 3 months.
- It is also recommended to take Vitamin K2 in the form of MK7. Recommended dose of 100 micro grams.
- Consider taking Melatonin at night 2mg.
- I like to add Omega 3 (DHA) fatty acid supplements 350 mg.
- Zinc (30 to 60 mg) is a great immune system support vitamin. It is hard to get into your cells because of its ion charge.
- Green Tea (polyphenol) aides in getting Zinc into your cells. I make it by boiling pure water with FRESH ginger root (a natural anti inflammatory), lemon and cinnamon sticks (a natural antibiotic) first. Add the green tea after you boil the other ingredients… Let the water cool a little before adding the leaves.
- Turmeric Curcumin Root is a natural anti-inflammatory 15 mg.
- Ginger Root Powder (from 10-1 concentrate) 1500 mg.
- Quinine. I take it in the form of tonic water. In the US Schweppes is a good choice. I drink several glasses a day. The best TONIC water in my opinion containing quinine is Fever-Tree out of India. It has higher levels of Quinine and less sugar. You can make your own Quinine by buying Cinchona bark purchased at the health food store and making your own. Lots of recipes on the internet.
- Nicotine. Despite the hysteria there are many known health benefits. Studies have show that Nicotine is a natural Ace2 inhibitor. And in your sinus it is an antiviral. I prefer to get my nicotine dose by smoking a pipe with organic tobacco filtered through a charcoal filter. Just like Bill Clinton I do not inhale. I now live a minimalist lifestyle with a few exceptions left over from my NY days. Every day I smoke 1 Cohiba Maduro 5 Magicos cigar. If your are nasty smoke obsessed you could consider using a nicotine patch or vaping pure nicotine diluted as per instructions… (Consult your Doctor). These patches and vaping can be dangerous.
- Mouthwash. I learned a long time ago to fight other corona viruses to OFTEN gargle with a mouth wash containing Chlorhexidine Digluconate. Most all the respiratory viruses grow in the case of the flu on the roof of your mouth. The Coronavirus grows in the back of your sinuses and then “leaks” into your throat and into your lungs. Many studies have show a benefit from vigorously gargling with the RIGHT mouth wash.
- Left over from a different time in my life is a passion for Scotch Whiskey. Now not just any Scotch but Macallan single malt 30 year old. I drink 1 fluid ounce every day after the markets close. The stuff costs silly money. But I have a stash in my “trophies case” See I get the stuff for free. I ask everyone who joins my Millionaires Club to send me a bottle. Needless to say I have a nice stash.
In closing we make no medical claims whatsoever for the above. These are suggestions I found in published research from what I regard as credible sources. In The Pandemic Informer news pages I have published the studies that support these conclusion. ThePandemicInformer.com Click the link and the page will open in a new browser tab. Call 866-924-0607 for a username and password.
Before taking any medicines, home remedies, vitamins or a drink of water consult your medical professional.
We make no medical claims nor allude to any medical benefit of or for the vitamins, minerals, supplements, tobacco products, mouth wash, whiskey or filters or mechanical devices mentioned in this report.
WARNING: Cigar smoking can cause cancers of the mouth and throat, even if you do not inhale.
WARNING: Pipe Tobacco contains nicotine. Nicotine is an addictive chemical.
WARNING: Vaping products contain nicotine. Nicotine is an addictive chemical.
All French regions placed on high virus alert – Macron
In a stark TV address to the nation, the French President warned: “The virus is circulating in France at a speed that even the most pessimistic forecasts had not anticipated.”We are all overwhelmed by a second wave which we know will arguably be tougher and more deadly than the first.”The new lockdown, which will run until December 1, will be reviewed every two weeks. It comes after 527 more deaths were recorded yesterday in France, the highest daily death toll since April, with 33,417 new confirmed cases in 24 hours. Under France’s new measures visits to care homes – which were banned during the country’s previous two-month lockdown – will still be allowed.
The virus is circulating in France at a speed that even the most pessimistic forecasts had not anticipated Emmanuel Macron
Mr Macron added: “If we do not put a brutal brake on contamination today, our hospitals will quickly become overwhelmed.”We will never let hundreds of thousands of our fellow citizens die. These are not our values.” Meanwhile, the EU’s top adviser on the pandemic warned most of the continent will have to go back into some form of lockdown. Professor Peter Piot said people had “relaxed too much” on social distancing measures like mask wearing and now “we’re paying a high price”.
And he warned if current restrictions are eased too soon Europe may face “a third wave with maybe even more deaths”. It comes as another 310 Brits were reported today to have died from coronavirus, as deaths double in just a fortnight. Brussels boss Ursula von der Leyen admitted Christmas will be “different” but said “a lot depends on behaviour from each individual in the next few weeks”. Mrs Merkel signed off on a second lockdown for all of November after an emergency meeting with state premiers from across Germany. She admitted: “We are now at a point where, on average nationally, we no longer know where 75 per cent of infections come from.”
We are now at a point where, on average nationally, we no longer know where 75 per cent of infections come from Angela Merkel
Under the measures, due to come in on Monday morning, people will be restricted to meeting members of just one other household in public. Bars, restaurants, gyms, and cultural venues will be ordered to close and hotels can only stay open for non-tourism related stays. Schools and nurseries will be allowed to stay open as will shops so long as they impose hygiene measures and limit customer numbers. The plan says: “Families and friends should be able to meet each other even under Corona conditions during the Christmas season.” In France, Mr Macron ordered bars, restaurants, and secondary schools to shutter as of midnight on Thursday. In France, schools and key public services were given a reprieve after doctors warned hospitals are just days from being overrun. Europe is being ravaged by a second wave of the virus that experts are warning will be worse than the first. Authorities in Belgium, which has the highest case rate in the EU, are also eyeing a second national lockdown as early as this weekend.